Topic Summary
By Center for Fluoride Research Analysis / Fluoride Science Editorial Board
Last updated: September 12, 2016
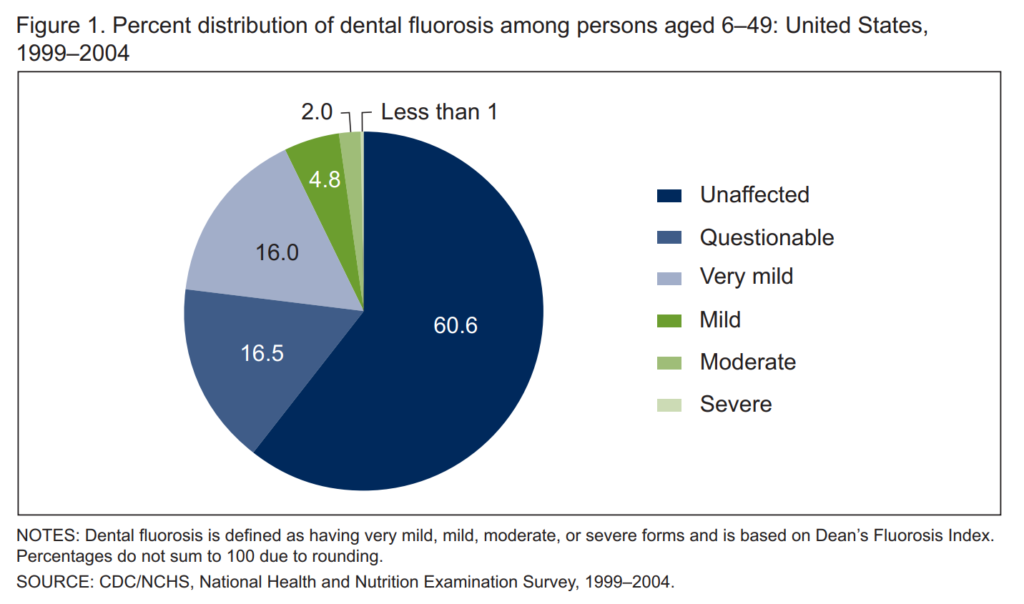
Enamel fluorosis, or dental fluorosis, is a hypomineralization of enamel that is characterized by greater surface and subsurface porosity than in normal enamel due to excessive intake of fluoride during tooth development, with a wide range of severity.1,2 Fluorosed surface enamel contains higher fluoride concentrations than does unaffected enamel, and teeth with fluorosis are more resistant to caries attack when compared to teeth without fluorosis.1,3 The milder forms of fluorosis on enamel appear as barely noticeable fine lacy/white markings and lines, while the severe form involves larger opacity along with pitting and roughness of the surfaces that allow staining after the tooth erupts into the mouth.1,4 According to the 1999-2004 National Health and Nutrition Examination Survey (NHANES) data, less than one quarter of persons aged 6-49 in the US had some form of dental fluorosis (23% prevalence). Very mild fluorosis was the most common form (16%) followed by mild (4.8%), moderate (2%), and severe (less than 1%) forms.4
Fluorosis is a dose-response condition, and the severity is dependent on the dose, duration, and timing of fluoride exposures.1,5,6 For the permanent teeth (except the third molars) the age at risk for enamel developing fluorosis is generally the first 8 years of life—Early-erupting teeth, such as maxillary central incisors, appear to be most susceptible to fluoride during the first 2-3 years, while late-erupting permanent teeth, such as canines, premolars, and second molars, may be at risk for fluorosis up to age 8 years.1,4-6 As to the dose of fluoride, defining a universally applicable upper limit of fluoride exposures to prevent unaesthetic enamel fluorosis is a challenge. The Institute of Medicine established a fluoride intake of 0.1mg/kg/day for children 0-8 years of age as a Lowest-Observed-Adverse-Effect Level (LOAEL) for moderate-severe forms of fluorosis in 1997, based on available cross-sectional data and experts’ consensus.7 However, the significance of exceeding this level with respect to the development of fluorosis is assumed to be influenced by various factors and should be evaluated with its timing and cumulative duration of exposure.
Reported risk factors for the development of fluorosis on enamel include drinking water with high natural fluoride levels, inappropriate use of fluoride supplements, fluoridated toothpaste, and/or exclusive consumption of infant formula reconstituted from fluoridated water (please see the topic summaries on fluoride toothpaste and infant formula for more information).1,2,8-11 While some reports indicate race/ethnicity as a potential demographic risk factor,1,2,12,13 the evidence of such relationship is mixed,11-14 and the cause, if any, is mostly unknown other than the potential influence of health behaviors such as infant feeding, fluid consumption, and the use of fluoride toothpaste on children’s exposures to fluoride.1,2,13,16
Since fluoridation of community water supplies began in the United States in 1945, the sources of both dietary and non-dietary (i.e. personal- or professional-use oral care products) fluoride have increased. The increased overall exposures to various sources of fluoride for children at the critical time of tooth development have resulted in an increase in the prevalence of dental fluorosis since Dean’s classic epidemiological studies in the 1930s.1-3,17 During this time there has also been a steep decrease in the caries experience among US children.1,2 The risks of fluorosis, thus, must be weighed against the known benefit of fluoride to prevent caries.
In April 2015, the US Department of Health and Human Services revised an earlier, climate-dependent recommendation for optimal fluoride level in drinking water, now recommending the concentration of 0.7 mg/L throughout the US.18 This standardized level of fluoride in drinking water maintains the public health benefit of caries prevention while reducing the likelihood of fluorosis. It is estimated that approximately 25% reduction in fluoride intake from drinking water alone and a reduction of approximately 14% in total fluoride intake may result from implementation of this new policy.18,19 In order to better monitor the prevalence of fluorosis, differentiating it from other developmental defects of enamel that manifest similar bilateral opacities, and the pattern fluoride exposures, the NHANES has started to collect detailed information of survey participants’ fluoride exposures since 2013.
The following section summarizes the findings from the most recent systematic reviews on this topic.
SYSTEMATIC REVIEWS THAT DISCUSS ENAMEL FLUOROSIS AND WATER FLUORIDATION
MCDONAGH ET AL (2000)20
Eighty-eight studies of fluorosis were included. These were largely cross sectional designs with only four controlled before-after designs. Despite the considerable heterogeneity between studies and low quality of evidence, authors reported that the prevalence of fluorosis is highly associated with the concentration of fluoride in drinking water. The pooled estimate of the prevalence of fluorosis at a water fluoride concentration of 1.0 ppm was 48% (95%CI 40%-57%) and for fluorosis of aesthetic concern 12.5% (95%CI 7.0%-21.5%).
NRC REPORT (2006)9
The committee reviewed scientific evidence on the occurrence of enamel fluorosis at fluoride concentration of 2mg/L and above to assess the adequacy of the US Environmental Protection Agency’s maximum-contaminant level goals (MCLG) of 4 mg/L and the secondary maximum contaminant level (SMCL) of 2mg/L of fluoride. One of the questions that this committee addressed was whether severe enamel fluorosis should be considered to be an adverse cosmetic effect or adverse health effect. While no new evidence suggested a link between severe dental fluorosis experienced in the US and a person’s ability to function, the committee acknowledged that severe fluorosis with discrete and confluent pitting compromises health-protective function of enamel by causing structural damage to the tooth and concluded that the MCLG should prevent the occurrence of this unwanted condition.
The reviewed evidence suggests that severe enamel fluorosis occurs at an appreciable frequency, approximately 10% on average, among children in US communities with water fluoride concentration at or near the current MCLG of 4mg/L. The prevalence of severe fluorosis is close to zero in communities at all water fluoride concentrations below 2mg/L (the current SMCL), while isolated cases could still occur from excessive fluoride exposure from other sources, such as toothpaste swallowing and use of fluoride supplements and rinses. One can also never rule out the possible existence of an individual’s hypersusceptibility to fluoride or the misdiagnosis of an enamel blemish as fluorosis, even if it is due to other causes.
IHEOZOR-EJIOFOR ET AL. (COCHRANE REVIEW 2015)21
The authors analyzed 90 studies and 40 studies, published between 1941 and 2014, for the effect of community water fluoridation on any level of fluorosis and aesthetic concerns of fluorosis, respectively, in the quantitative syntheses. In line with the previous systematic review (by McDonagh 2000), primary analysis was carried out on data where fluoride exposure was 5ppm or less. The authors found over 97% of the studies to be at high risk of bias and substantial between-study variation. The effect of fluoride exposure was found to be positive and statistically significant in all models of analyses, and a higher prevalence of dental fluorosis is associated with increased fluoride exposure. They found that at a fluoride level of 0.7ppm, the percentage of participants with fluorosis of aesthetic concern was approximately 12% (95%CI 8% to 17%; 40 studies, 59,630 participants) and percentage with any level of fluorosis was 40% (95% CI 35% to 44%) (detected under highly controlled, clinical conditions; 90 studies, 180,530 participants).
REFERENCES
- Burt BA, Eklund SA. Dentistry, Dental Practice, and the Community. 6th St Louis: Elsevier Saunders; 2005
- Beltran-Aguilar ED, Barker LK, Cantro MT et al. MMWR Surveill Summ. 2005;54(3):1-44 https://pubmed.ncbi.nlm.nih.gov/16121123/
- Iida H, Kumar JV. The association between enamel fluorosis and dental caries in US school children. JADA. 2009;140:855-62
- Beltran-Aguilar ED, Barker LK, Dye BA. Prevalence and severity of dental fluorosis in the United States, 1999-2004. NCHS Data Brief. November 2010; No. 53.
- Hong L, Levy SM, Broffitt B et al. Timing of fluoride intake in relation to development of fluorosis on maxillary central incisors. Community Dent Oral Epidemiol. 2006;34:299-309
- Bhagavatula P, Levy SM. Broffitt B et al. Timing of fluoride intake and dental fluorosis on late-erupting permanent teeth. Community Dent Oral Epidemiol. 2016;44:32-45
- Institute of Medicine. Dietary reference intakes for calcium, phosophorus, magnesium, vitamin D, and fluoride. Washington, DC. National Academies Press. 1997.
- Pendrys DG, Katz RV, Morse DE. Am J Epidemiol. 1994;140:461-71 https://pubmed.ncbi.nlm.nih.gov/8067338/
- Pendrys DG, Katz RV, Morse DE. Am J Epidemiol. 1996;143:808-15 https://pubmed.ncbi.nlm.nih.gov/8610691/
- National Research Council. Fluoride in Drinking Water: A Scientific Review of EPA’s Standards. Washington, DC. The National Academies Press. 2006.
- Hujoel PP, Zina LG, Moimaz SAS et al. Infant formula and enamel fluorosis- A sustematic review. JADA. 2009;140(7):841-54
- Kumar JV, Swango PA. Low birth weight and dental fluorosis: is there an association? J Public Health Dent. 2000;60(3):167-171
- Martinez-Mier EA, Soto-Rojas AE. Differences in exposure and biological markers of fluoride among White and African American children. J Public Health Dent. 2010;70(3):234-40
- Franzolin Sde O, Goncalves A, Padovani CR et al. Epidemiology of fluorosis and dental caries according to different types of water supplies. Cien Saude Colet. 2010;Jun;15 Suppl 1:1841-7
- Arora S. Enamel fluorosis among different racial/ethnic groups in U.S. school children. Abstract from the 2016 National Oral Health Conference.
- Heller KE, Sohn W, Burt BA et al. Water consumption and nursing characteristics of infants by race and ethnicity. J Public Health Dent. 2000;60(3):140-6
- Dean HT. Classification of mottled enamel diagnosis. J Am Dent Assoc. 1934;21:1421-6.
- S. Department of Health and Human Services Federal Panel on Community Fluoridation. U.S. Public Health Service Recommendation for Fluoride Concentration in Drinking Water for the Prevention of Dental Caries. Public Health Reports. Jul-Aug 2015. Vol.130 Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4547570/
- Environmental Protection Agency. Fluoride: exposure and relative source contribution analysis. Washington: EPA, Office of Water, Health and Ecological Criteria Division; 2010.
- McDonagh MS, Whiting PF, Wilson PM, Sutton AJ, Chestnut I, Cooper J et al. Systematic review of water fluoridation. Br Med J. 2000;321:855-9.
- Iheozor-Ejiofor Z, Worthington HV, Walsh T, et al. Water fluoridation for the prevention of dental caries. Cochrane Database Syst Rev. 2015, June 18. Abstract available at https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010856.pub2/epdf/abstract
Other resources
| Putting Fluorosis in Context | Interview with Dr. Steven Levy |
